Granger was an 11 y FS DMH who presented to our Internal Medicine service for weight loss and nasal signs. Her owners reported that her sneezing, congestion, and loud breathing had gotten progressively worse over the past year. In the past few months she had a few episodes of bloody nasal discharge and sneezing fits. She became very picky about which foods she would eat at home. She had previously been placed on oral antibiotics for suspected chronic rhinitis, but they had only temporarily improved her clinical signs.
On physical examination she has a thin body condition, was stertorous, and had evidence of nasal congestion. A CBC, chemistry, and T4 were unremarkable. Thoracic radiographs revealed only aerophagia (suspected to be secondary to severe nasal disease) but was otherwise unremarkable. An abdominal ultrasound was unremarkable. Granger was admitted to the hospital for a head CT and rhinoscopy with Dr. Sarah Noble for continued investigation into the cause of his clinical signs.
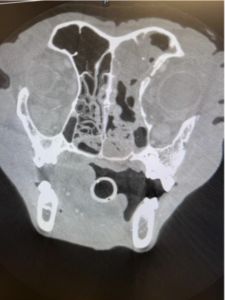
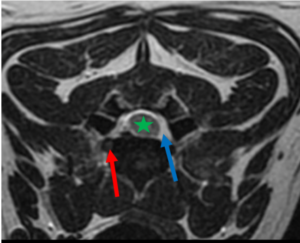
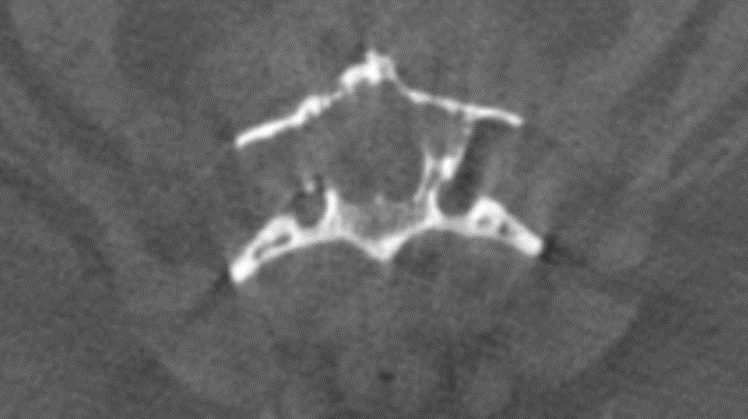
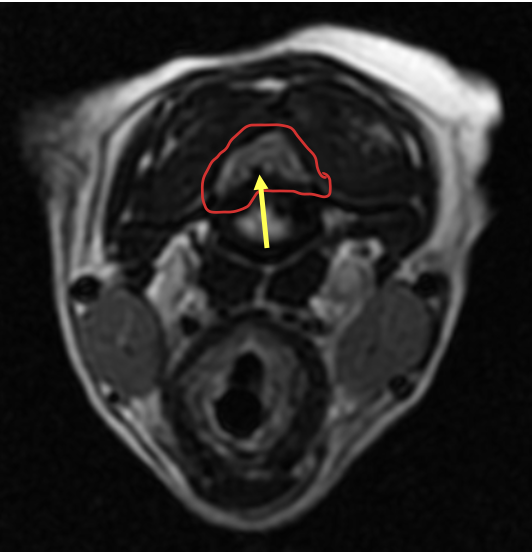
Her head CT revealed a large peripherally contrast-enhancing and irregularly marginated ovoid mass filling the nasopharynx and middle ear. There were multiple areas of lysis associated with the osseous bulla, and secondary obstructive rhinitis was suspected. The medial retropharyngeal lymph nodes were mildly enlarged, which was suspected to be due to reactive hyperplasia. Differentials for this type of mass on CT include carcinoma vs fungal disease (cryptococcus) vs a chronically infected nasopharyngeal polyp with concurrent otitis media/interna.
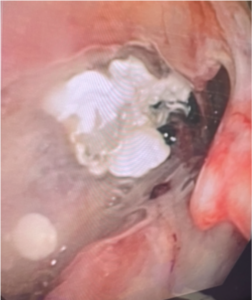
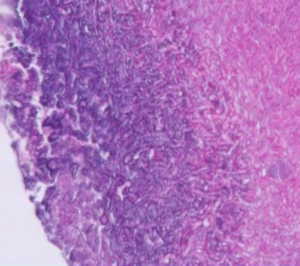
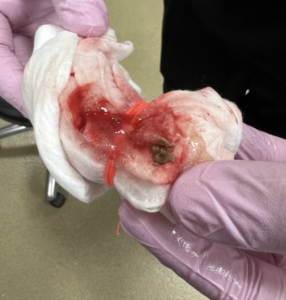
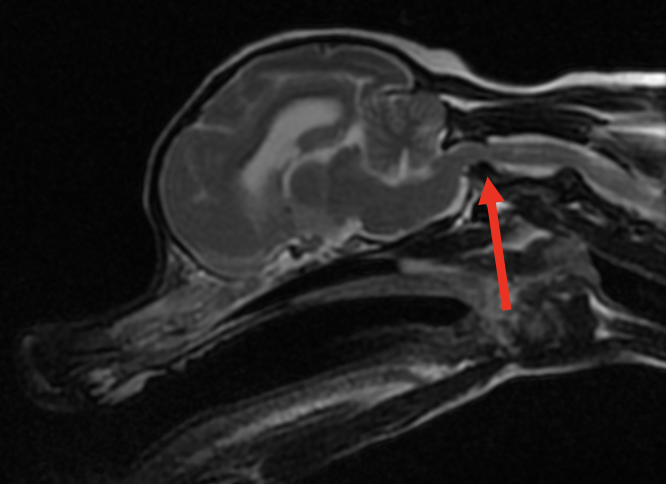
Dr. Noble removed the large, irregular looking mass from the nasopharynx under general anesthesia. A polyp vs neoplasia was prioritized based on the appearance of the mass. There was mild bleeding with some draining purulent material following mass removal, but Granger’s recovery from general anesthesia was uneventful. The mass was submitted for histopathology, and the pathologist confirmed her mass was an “ulcerated and severely inflamed benign feline nasopharyngeal polyp”. As of the publication of this article she has continued to do well at home.
CLINICALLY RELEVANT FACTS:
- Feline nasopharyngeal polyps should be considered a differential for chronic nasal signs in cats, despite their age.
- In cat’s with this condition surgical removal can be curative, however regrowth of the mass occurs in some patients which may require additional treatment. A ventral bulla osteotomy will often be recommended in these cases. It has previously been reported in the literature that 50% of polyps will regrow in feline patients.
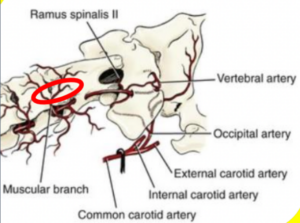
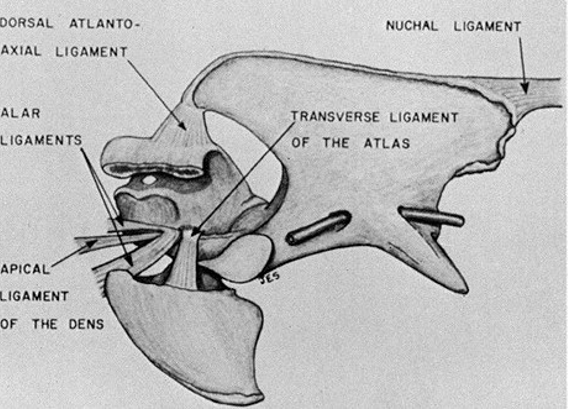
- Removal of the polyp will often lead to Horner syndrome (oculosympathetic dysfunction) on the side of the polyp’s origin. Owners should be warned about the potential of polyp regrowth, as well as the risk of Horner syndrome which may not resolve.
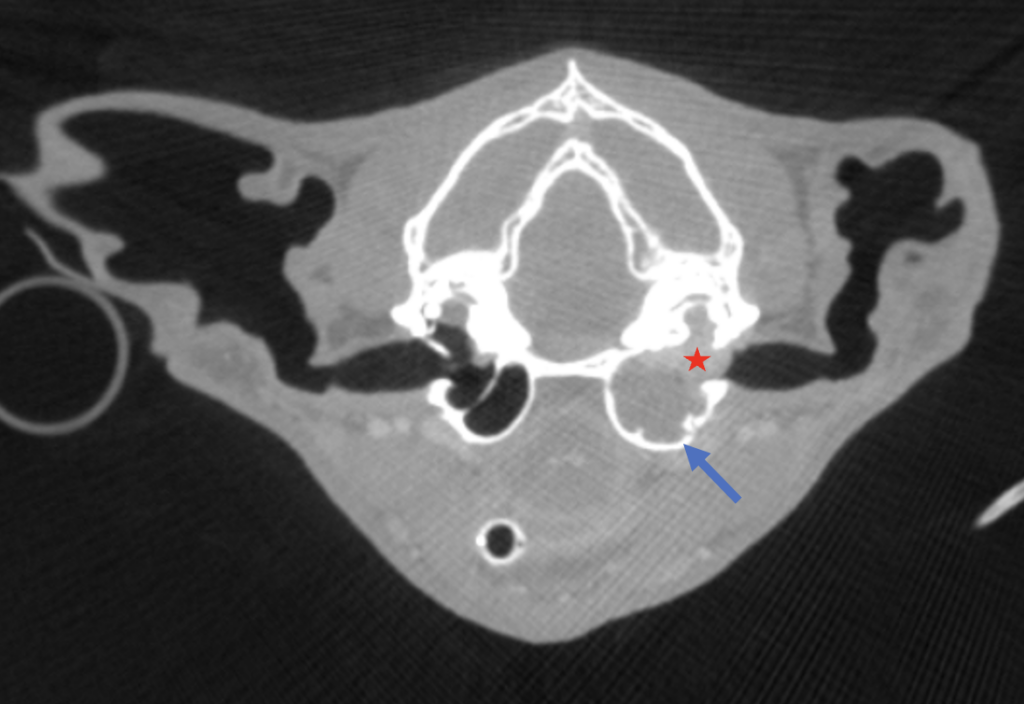
The red star shows the contrast enhancing mass seen in the left nasopharynx and middle ear. The left osseous bulla (blue arrow) is thin, expanded compared to the right, and has areas of bony lysis.

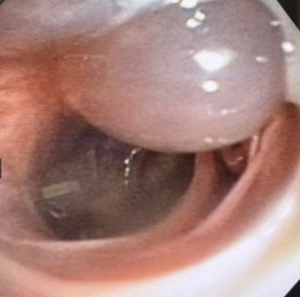
The nasopharyngeal polyp is visible as Dr. Noble applies gentle traction.
Granger had left Horner syndrome (left ptosis, miosis, enophthalmos, and third eyelid elevation) following the procedure.

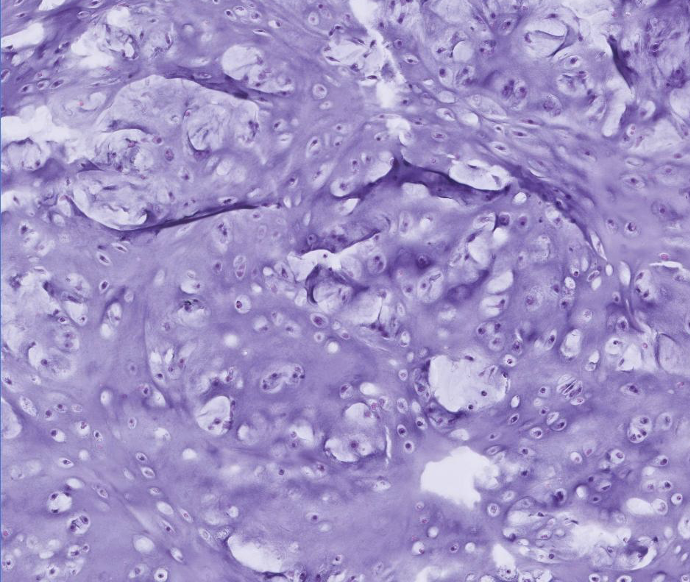
The irregularity of the mass was concerning for neoplasia, but was ultimately due to chronic ulceration and inflammation.
Authored by: Dr. Landry, DVM, DACVIM, Neurology
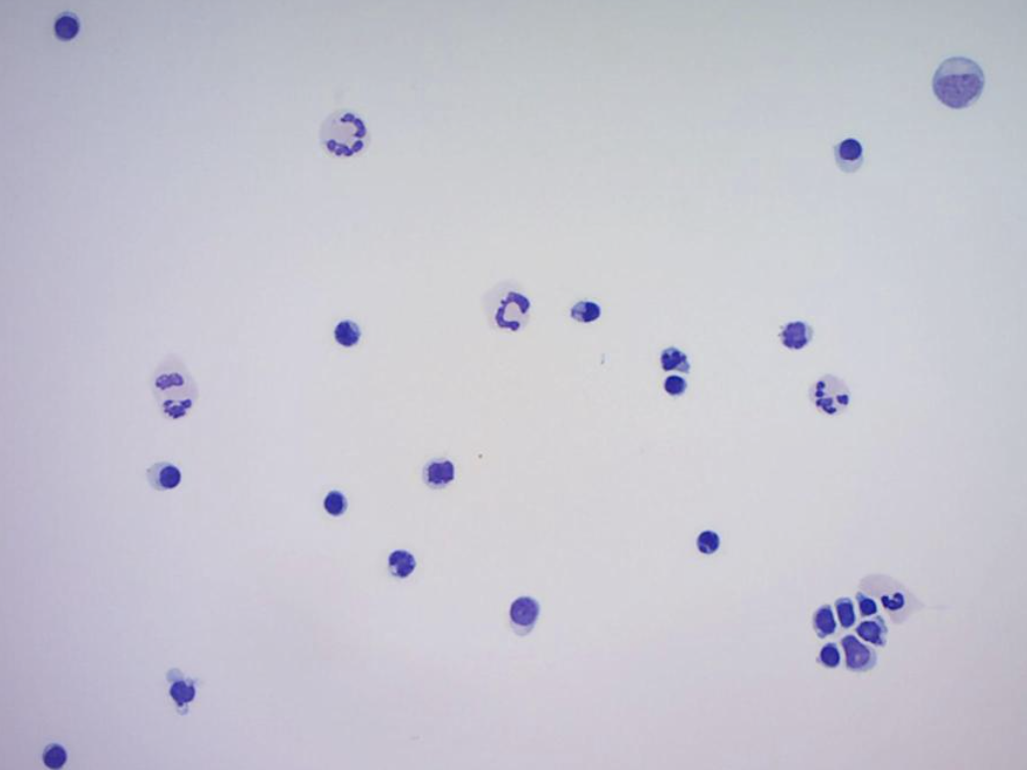
 In June 2023, Lucy was presented to her primary care veterinarian for lethargy and left-sided facial swelling. The owner elected to treat empirically for an infectious/inflammatory process with antibiotics and a non-steroidal anti-inflammatory medication. Lucy initially had a favorable response to empirical therapy, but the swelling returned in October 2023. Lucy was evaluated by her primary care veterinarian who appreciated generalized peripheral lymphadenopathy during her exam. Bloodwork revealed a non-regenerative anemia (26.1%), lymphocytosis (8.97K), monocytosis (3.18K), thrombocytopenia (97K) and elevated ALP (459). Cytology of her lymph node was most consistent with a diagnosis of large cell lymphoma and she was referred to PVESC at that time.
In June 2023, Lucy was presented to her primary care veterinarian for lethargy and left-sided facial swelling. The owner elected to treat empirically for an infectious/inflammatory process with antibiotics and a non-steroidal anti-inflammatory medication. Lucy initially had a favorable response to empirical therapy, but the swelling returned in October 2023. Lucy was evaluated by her primary care veterinarian who appreciated generalized peripheral lymphadenopathy during her exam. Bloodwork revealed a non-regenerative anemia (26.1%), lymphocytosis (8.97K), monocytosis (3.18K), thrombocytopenia (97K) and elevated ALP (459). Cytology of her lymph node was most consistent with a diagnosis of large cell lymphoma and she was referred to PVESC at that time. Figure 1. VD pelvis showing significant hip dysplasia bilaterally with secondary degenerative changes prior to a year of age
Figure 1. VD pelvis showing significant hip dysplasia bilaterally with secondary degenerative changes prior to a year of age







 Junior was presented to our Oncology service for consultation following a diagnosis of cutaneous hemangiosarcoma made via biopsy of a mass removed by his primary care veterinarian. The mass had been present for about 4 months and started to grow rapidly leading up to its removal. Histopathology of the mass was most consistent with a diagnosis of cutaneous hemangiosarcoma. Unfortunately, invasion into subcutaneous tissue was observed and complete excision could not be confirmed. Both variables have been associated with an unfavorable prognosis.
Junior was presented to our Oncology service for consultation following a diagnosis of cutaneous hemangiosarcoma made via biopsy of a mass removed by his primary care veterinarian. The mass had been present for about 4 months and started to grow rapidly leading up to its removal. Histopathology of the mass was most consistent with a diagnosis of cutaneous hemangiosarcoma. Unfortunately, invasion into subcutaneous tissue was observed and complete excision could not be confirmed. Both variables have been associated with an unfavorable prognosis.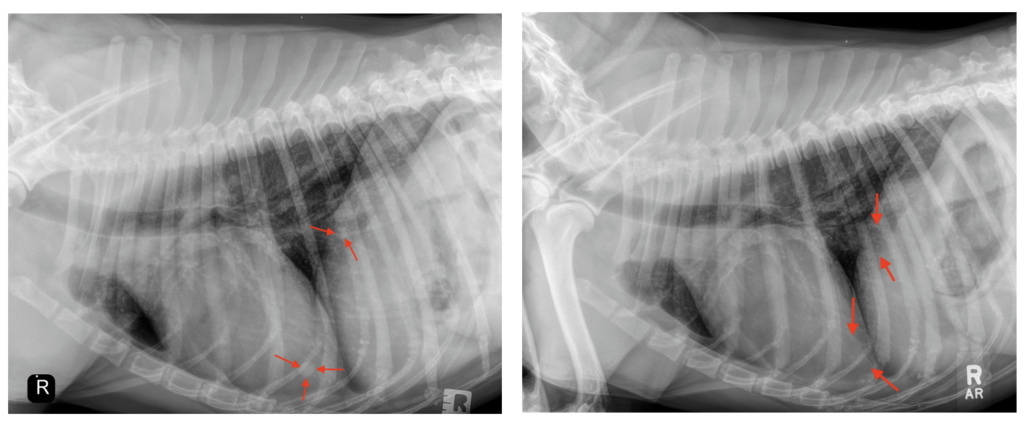
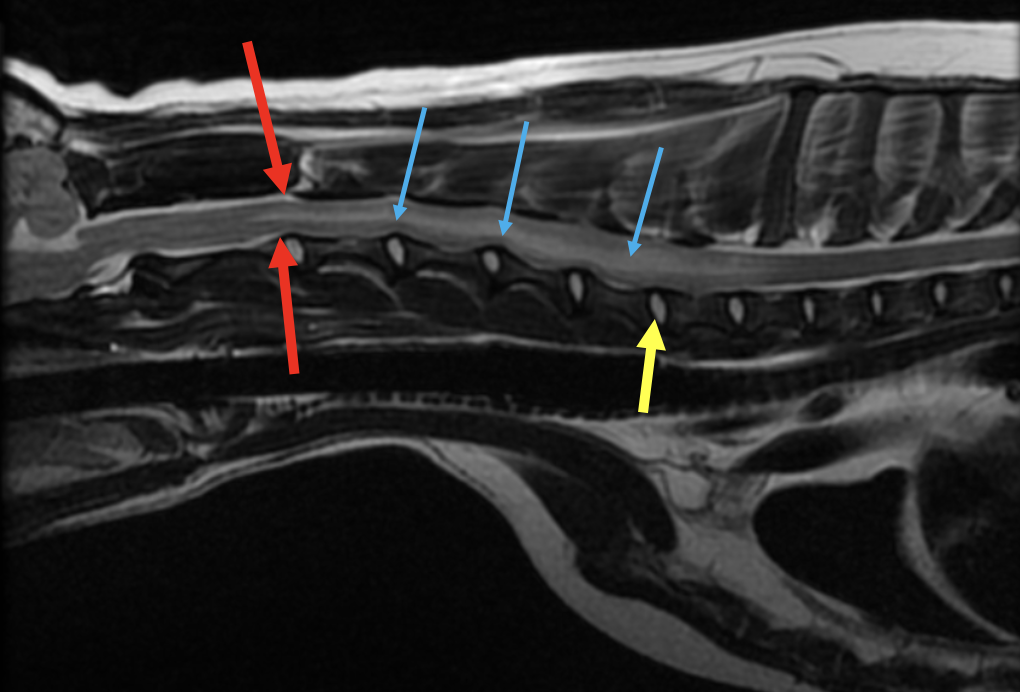
 Opal is a 1.5 year SF Pit Bill Mix who presented to our Neurology service for a one-week history of dragging her pelvic limbs intermittently. Opal first started showing symptoms after running in the woods with her housemates. That evening she began limping in her pelvic limbs, and since then Opal had been only able to walk about 30 feet before she would start to drag her pelvic limbs behind her. Her owners report that with a period of rest she is able to get up in her back legs to attempt to walk again. Over the past few days she developed diarrhea and has not been eating well. A CBC, 4DX, and radiographs of the abdomen/thoracolumbar spine were unremarkable at the emergency veterinary hospital. Due to concern for back pain she was started in carprofen, methocarbamol, metronidazole, and gabapentin which did not improve her signs.
Opal is a 1.5 year SF Pit Bill Mix who presented to our Neurology service for a one-week history of dragging her pelvic limbs intermittently. Opal first started showing symptoms after running in the woods with her housemates. That evening she began limping in her pelvic limbs, and since then Opal had been only able to walk about 30 feet before she would start to drag her pelvic limbs behind her. Her owners report that with a period of rest she is able to get up in her back legs to attempt to walk again. Over the past few days she developed diarrhea and has not been eating well. A CBC, 4DX, and radiographs of the abdomen/thoracolumbar spine were unremarkable at the emergency veterinary hospital. Due to concern for back pain she was started in carprofen, methocarbamol, metronidazole, and gabapentin which did not improve her signs.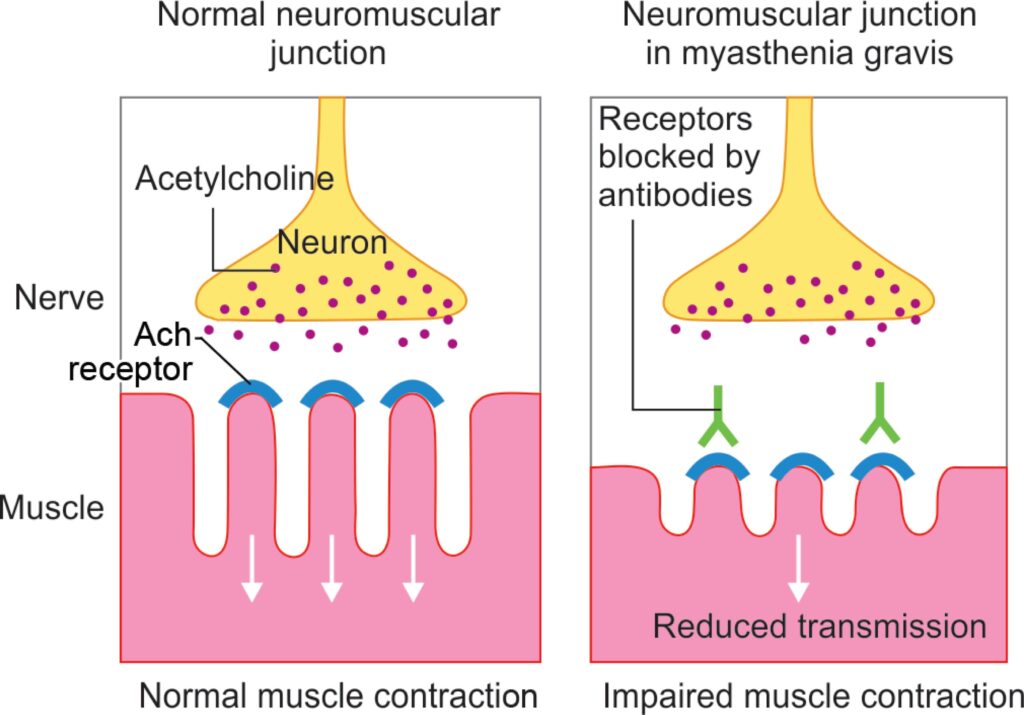

 The pathophysiology of smoke inhalation is multifactorial. The progression of clinical signs and prognosis differ depending on present respiratory irritants, thermal heat exposure, particulate matter size, and systemic toxins.
The pathophysiology of smoke inhalation is multifactorial. The progression of clinical signs and prognosis differ depending on present respiratory irritants, thermal heat exposure, particulate matter size, and systemic toxins.